Vaccines in the spotlight Understand article
Hit me with your best shot: Vaccines have taken centre stage in the COVID-19 pandemic. What are the different types and how do they work?
How do our bodies fight infections?
Microorganisms, like viruses or bacteria, that can cause disease when they enter our bodies are called pathogens. Our immune system fights against these pathogens and the B-cells of the adaptive immune system play a key role. They produce proteins called antibodies, which bind to specific parts of the pathogen called antigens and tag them for other immune cells to eliminate. Once B-cells and antibodies have been developed for a particular pathogen, they continue to scan the body to detect and attack it if it invades again.
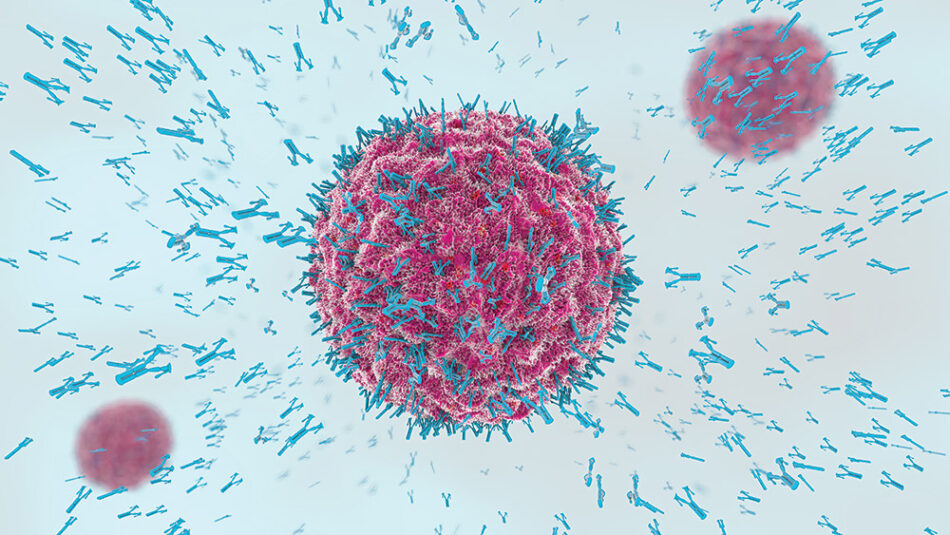
Image: Christoph Burgstedt/Shutterstock.com
Adaptive immunity is why people are able to recover from infections and usually don’t get sick with the same disease, like chickenpox, twice. However, some pathogens can trick our immune system and cause illness more than once. For example, the influenza virus mutates quickly, and new strains have different antigens that the immune cells and antibodies don’t recognize. Some other pathogens, like Mycobacterium tuberculosis (which causes TB) and human immunodeficiency virus (HIV), hide inside host cells where the immune system can’t find them.
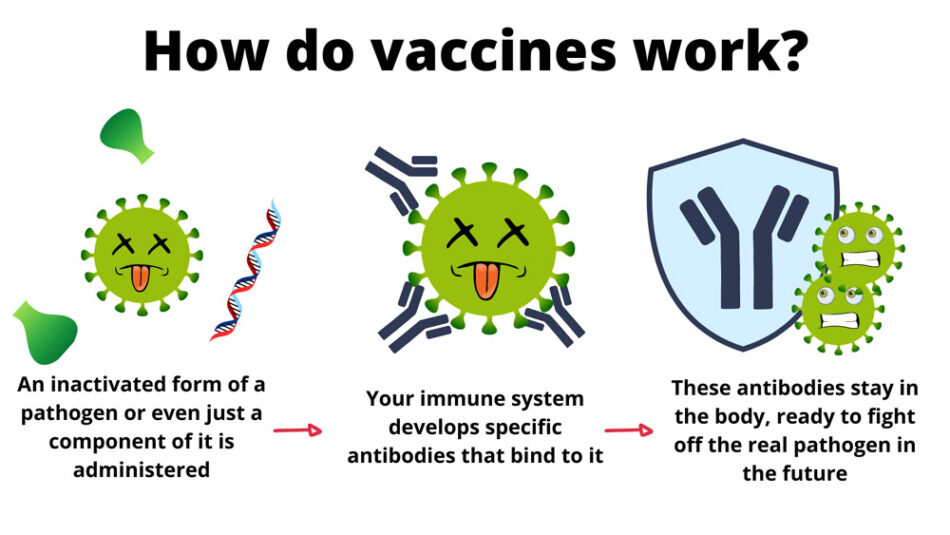
How do vaccines work?
Vaccines trigger the adaptive immune response in the same way that pathogens do but without the risks of getting an infection. They don’t make us sick because they contain modified or weakened pathogens or just the antigen part. However, your immune system still develops specific B-cells and antibodies, which will attack the real pathogen if it ever enters the body.
There are a number of vaccine development strategies, which lead to different types of vaccine.[1]
| Vaccine type | Contains | Examples |
|---|---|---|
| Live-attenuated | Weakened live pathogen | Typhoid fever, Measles, Mumps |
| Inactivates | Dead or inactivated pathogen | Influenza, Hepatitis A |
| Toxoid | Inactivated toxin from the pathogen | Diphtheria, Pertussis, Tetanus |
| Subunit | A part of the pathogen (antigen) | Hepatitis B, Typhoid fever |
| Nucleic acid | A genetically encoded antigen | Ebola, COVID-19 |
When choosing a strategy, several aspects need to be considered, such as:
- Can it safely be given to people with weakened immune systems?
- Is one dose (or set of doses) enough or are later booster shots needed to maintain immunity?
- What are the side effects?
- Does the vaccine need special storage, like very cold temperatures?
Every developed vaccine behaves slightly differently and must be carefully tested, but the different types also have some general properties to be considered.
Live, attenuated vaccines
These contain a weakened pathogen that doesn’t cause disease in healthy people.
- Advantages: contain many antigens and trigger a strong immune response; one or two doses usually enough for life-long protection
- Disadvantages: may cause more side effects; not safe for people with weakened immune systems; storage can be challenging
Inactivated vaccines
These use a dead or inactivated form pathogen.
- Advantages: safe for people with weak immune systems
- Disadvantages: may provide weaker protection than live attenuated vaccines; booster shots may be needed
Toxoid vaccines
These are based on the toxins produced by bacteria, which can be peptides, proteins, or other molecules. The toxoid is a modified toxin that is not as dangerous but provokes the same immune response.
- Advantages: no pathogen, so safe for people with weak immune systems
- Disadvantages: booster shots needed; not suitable for viruses (they don’t produce toxins)
Subunit vaccines
These contain only an antigen instead of the whole pathogen.
- Advantages: strongly activates the immune response; safe for people with weak immune systems
- Disadvantages: booster shots needed; can be difficult to isolate specific antigens that induce sufficient immune response
Nucleic acid vaccines
This newer technology uses genetic material – a small piece of mRNA or DNA – that contains instructions for human cells on how to make a protein (antigen) from the pathogen. These vaccines do not modify our DNA; after the antigen is produced by our cells, the small piece of vaccine DNA/RNA breaks down.
- Advantages: Can be quickly adapted for new pathogens and produced on a large scale; ideal for new or quickly mutating pathogens
- Disadvantages: Some RNA vaccines need to be stored at –20oC or –70oC; booster shots might be required
A subtype, the viral-vector vaccine, uses a modified carrier virus (vector) to transport the nucleic acid sequences of the target virus into our cells. These viral vectors are modified so that they can’t replicate in our bodies; they just transport the vaccine DNA/RNA and then break down.
Most newer-generation vaccines require a booster shot, however this is mostly a logistical issue and these vaccines still provide strong protection.
| Vaccine type | COVID-19 vaccine |
|---|---|
| Inactivated virus vaccine | Sinopharm, SinoVac |
| Viral vector vaccine | Sputnick V, Johnson & Johnson, AstraZeneca |
| mRNA-based vaccine | BioNTech/Pfizer, Moderna |
Vaccine development
Not every vaccination strategy works against every disease, and there are still no approved vaccines available against some pathogens, such as HIV. There is always an element of luck involved, and the time needed to develop a new vaccine can vary widely.
For the measles vaccine, the creation of the weakened virus – only the first step in development – took 10 years. For typhoid fever and Hepatitis B, it took around 100 and 15 years to develop the first vaccines.[2] The fastest any vaccine had previously been developed was four years for mumps; this record was broken by the development of COVID-19 vaccines in under a year.
This very short development time and the fact that they are the first approved mRNA vaccines have generated doubts in some people: why was it so quick and is the new technology safe? However, there are several reasons why it was possible for the COVID-19 vaccines to be developed so fast without compromising safety:
- Scientists have been working on developing mRNA vaccines for decades.[3] Improving stability and devising a method to get mRNA into cells was a long process but because this technology was already close to being ready, adapting it for SARS-CoV-2 was quick.
- In the global emergency of the COVID-19 pandemic, thousands of researchers around the world cooperated to find a solution. Furthermore, enormous governmental funding was invested, and although all of the normal regulatory tests were done, some were run in parallel rather than one after another to save time.[2]
- Prior work with similar coronaviruses that cause the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) also helped in the development of vaccines against COVID-19.
What is herd immunity?
When most of a population becomes immune to a pathogen, those who are not immune are also protected because people with immunity usually don’t spread the infection. This effect is called herd immunity and depends on the contagiousness of the disease: the easier the disease spreads, the higher the percentage of the population that needs to be immune to protect everyone. There are two ways to achieve herd immunity: through infection (natural immunity) or vaccination. The problem with natural immunity is that people have to actually catch the disease, which in some cases can be dangerous or even deadly.
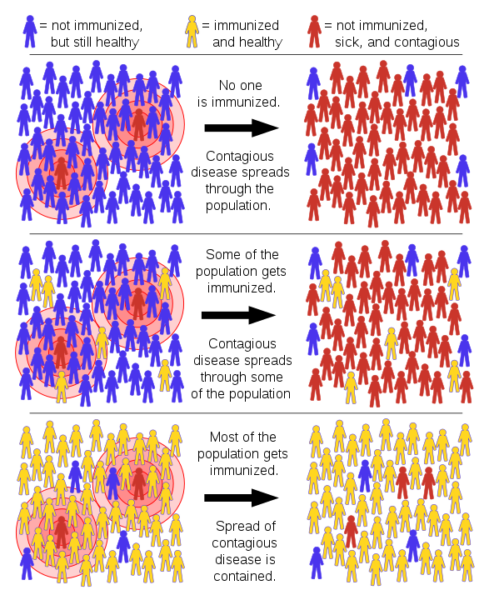
Image: Tkarcher/Wikimedia, CC BY-SA 4.0
The spread of many infectious diseases, like measles, mumps, polio, and chickenpox, has been effectively halted by vaccination and herd immunity. However, this does not mean that vaccination for these diseases can stop. If the vaccination rate decreases, herd immunity will disappear and new outbreaks will occur, like with measles in the USA in 2019.[4]
It is important to understand that only the development of targeted antibodies through vaccination (or infection) can reliably protect you against catching an infectious disease. Despite the advertising claims made by some companies about ‘natural immune-boosting remedies’, these do not provide real protection.[5,6]
References
[1] Information about types of vaccines on the Vaccine Knowledge Project website by the University of Oxford: https://vk.ovg.ox.ac.uk/vk/types-of-vaccine.
[2] An article on how the development of the COVID-19 vaccine could change future research in this Nature feature article: https://www.nature.com/articles/d41586-020-03626-1.
[3] A video on the research behind the development of the COVID-19 vaccine: https://youtu.be/XPeeCyJReZw.
[4] An article on herd immunity from the John Hopkins Bloomberg School of Public Health: https://www.jhsph.edu/covid-19/articles/achieving-herd-immunity-with-covid19.html.
[5] A BBC news article on why immune-boosting remedies don’t work: https://www.bbc.com/future/article/20200408-covid-19-can-boosting-your-immune-system-protect-you.
[6] An article from Slate on why boosting the innate immune system would be a bad idea: https://slate.com/technology/2014/12/boost-your-immunity-cold-and-flu-treatments-suppress-innate-immune-system.html.
Resources
- Watch a video on innate and adaptive immunity.
- Read about the history of vaccines.
- Learn more about how diseases spread: Kucharski A, Wenham C, Conlan A, Eames K (2017) Disease dynamics: understanding the spread of diseases. Science in School 40:52–56.
- Watch an engaging set of videos on mRNA vaccines and the science behind the COVID-19 vaccines.
- Watch a video that demonstrates how herd immunity works using mousetraps.
- Find additional resources on the COVID-19 vaccine on the Center for Disease Control and Prevention (CDC) website.
- Take a closer look at the COVID-19 mRNA vaccines on the CDC website.
Review
For more than one year the whole planet mourned and still mourns millions of people dying from virus infection. All of us lived and some still live tough lockdowns with all their negative effects on people and on their lives. All of us were, some still are, concerned about the new mRNA vaccines, how safe they are, or if we should be or not vaccinated.
Misunderstandings must be cleared so ignorance can and must be replaced with scientific knowledge. The average life expectancy has increased in the last decades and one of the reasons is population vaccinations. We must understand that science was and still is crucial in optimizing human’s life quality.
Alina Giantsiou – Kyriakou, Biology teacher, Kykkos B’ Lyceum Nicosia, Cyprus





